Life After COVID
– by J.E. Barnard
A reprint from the Dundurn Press blog of December 1, 2020
Sometimes when life and art overlap, it’s a happy
synchronicity. Other times not so happy, as when a friend experiences an
over-long recovery from COVID and her doctor has nothing to suggest. She typed,
“We can’t garden without needing naps; we can’t take walks; even grocery
shopping leaves us all exhausted for days. You know about managing fatigue from
your character Jan in those Falls books. Can you suggest anything we can try?”
I know about managing excessive fatigue not only because my character Jan has it
but because I have it too. Like an estimated 580,000 Canadians with ME/CFS [in January 2023 that number has increased significantly]. I
am intimately acquainted with the crushing exhaustion that overwhelms the body,
the brain, the spirit after the slightest exertion. It’s known colloquially as
‘the crash’, in the medical literature as Post-Exertional
Neuro-Immune Exhaustion (PENE) or Post-Exertional Malaise (PEM). It hits
whenever you over-use muscles, brain – even eyes or ears – beyond today’s
available energy (which may be different than yesterday’s or tomorrow’s).
Dr. Anthony Fauci, one of the USA’s top infectious disease experts, early warned of the danger of runaway post-viral syndrome leading to ME/CFS. ME experts recognized it too: COVID could lead to a spike in ME/CFS diagnoses around the world.
Why are they alarmed?
Well, 75% of people diagnosed with ME/CFS become too consistently unwell to return to their old jobs; most can’t consistently work even at home. 25% worldwide have such severe illness that they live in darkened rooms, unable to tolerate light, sound, touch. The worst-off can no longer digest food; they’re tube-fed or on IV nutrients for years on end. The majority of their care needs fall on their family members, taking more people out of the workforce and eating through a family’s savings.
Nearly nine months into the pandemic, “longhaulers” are turning up in online ME/CFS groups around the world, looking for tips on managing the debilitating exhaustion, pain, and brain fog. Up to 30% of those who recover from the active phase of COVID – many of whom had only mild illness at the time – remain stricken by fluctuating symptoms that severely affect their daily activities including work, grocery shopping, housecleaning, and anything recreational. Some need home-care services now, even though they weren’t ‘that sick’ while they were officially ill with COVID. [here's a 2023 research summary that reveals just how damaging even a single COVID infection can be to your organs, immune system, blood clotting]
Even if only 10% of the world’s millions of COVID cases turn into Long-COVID, this is a looming disaster for patients, for health services, and for the economy.
In the USA, Dr. Mady Hornig, an ME expert at Columbia University in New York, is still recovering from her bout of COVID last spring. To say she’s worried about the potential disaster of Long COVID would be an understatement. She discusses her own illness experience and her work on ME/CFS with a panel for This Week In Virology . If you don’t have the time or the mental focus to watch the whole hour-plus discussion, you can find some of her comments in this recent Columbia Magazine article.
Here in Canada, Dr. Alain Moreau of Montreal’s ME / CFS Collaborative Research Center (under the Canadian Institutes of Health Research, or CIHR) started blood-sampling COVID patients last spring, proactively tracking them through their recoveries in hopes of identifying the biochemical twists that turn COVID into Long COVID, and possibly into ME/CFS. The clues provided may lead to treatments for both illnesses.
While Long COVID is not so far shown to be biochemically identical to ME/CFS, my afflicted friend and countless others are finding symptomatic help via the self-management strategies used by ME/CFS patients: splitting tasks into smaller increments, assertively resting before they feel tired, and monitoring their heart rate during activites for a clear signal when to stop.
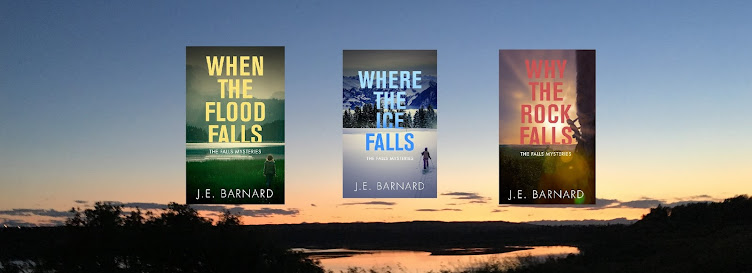
After three months of this regimen my friend reported she’s gradually increasing her daily activities and only sporadically having symptom recurrence. She’s not cured but she’s got hope again...like my character Jan in Why the Rock Falls, but minus Jan’s involvement with missing persons, murder, and some fabulous historical artworks of the Rocky Mountains.
If you’re stuck at home recovering from COVID, out in the world trying to avoid catching it, or exposed and isolating to protect those more vulnerable, you can follow links throughout this blog to resources on both Long COVID and ME/CFS. You can also escape COVID news by following Jan and Lacey through another deadly adventure in their idyllic foothills town.
Stay safe, stay calm, stay kind, and please wear a mask wherever indicated. Even if you think you’ll fight off the virus just fine, you could end up in that 30% for whom the virus is only the beginning.
[Check out my ME/CFS page for more self-care resources, including some newly added from the past 2 years of Long COVID research]